Physiotherapy for Vestibular Rehabilitation
Assessment
Physiotherapist’s play a key role in the assessment and diagnosis of patient’s with vestibular conditions; often being one of the first health professionals to see them. Therefore, it is crucial that a thorough assessment is completed to facilitate the best outcomes for the patient (Derebery, 1999; Parnes, Agrawal, & Atlas, 2003).
Subjective
It’s important that the therapist gains a good background before performing any objective tests. The subjective interview for vestibular conditions is similar to that of any other condition, with some added questions that need to be asked. A good subjective interview should include:
-
History of presenting condition - a detailed description of the presenting condition
-
Previous episodes - has the patient experienced these symptoms before? If so, When? For how long? How was it treated?
-
Date of onset - when the symptoms started
-
Description of dizziness (tumbling/spinning/vertigo) - does the patient feel as though they are spinning or the world is spinning around them?
-
Aggravating factors - rolling L/R, lying down L/R/backwards, bending over, looking up, turning, stairs, ADLs etc.
-
Easing factors - as above
-
Duration - how long do episodes last for?
-
Intensity - ask the patient to give a rating of symptoms out of 10 and whether intensity is improving or getting worse since onset
-
Frequency of symptoms - how many episodes does the patient experience throughout the day?
-
24 hour behaviour - how do the symptoms change throughout the day? Are they worse at any particular time?
-
Nausea - are they experiencing nausea?
-
Decrease concentration/fatigue - has the patient experienced a decrease in concentration and/or increase in fatigue?
-
Vision - diplopia and/or blurred vision? Does the patient wear corrective glasses? Last eye test? Issues with depth perception? Difficulty seeing in dim light?
-
Hearing - Experiencing loss of hearing, tinnitus and/or fullness in ear?
-
Nutrition - In general how is their diet? And have there been any changes lately?
-
Past medical history - patient’s medical history
-
Falls history - has current condition increased falling or unsteadiness?
-
Medication - list of current medications. Any recent changes to medication? Are they taking medication for current condition? If so, is it helping?
-
Investigations - have they had any investigation?
-
Social history - including who patient lives with, supports, home set-up, employment, recreation and driving
-
Pre-morbid mobility - what was the patient’s PMM and has it changed?
Oculomotor Assessment
The following are objective tests that are used to assess and diagnose pateint's with vestibular conditions (Newman-Toker, 2012; Price Alexander Hospital, 2014).
Smooth Pursuit Test:
Procedure:
1. Instruct patient to keep head still.
2. Ask patient to follow your finger/pen (keeping it about 60cms away from the patient’s face) while you move your finger/pen 30 degrees to the left, right, up and down.
3. Pause in each position to observe nystagmus, note direction.
Look for:
-
Smooth conjugate eye movement.
-
Abnormal is jerky (or saccadic) eye movement. Note the direction of pursuit when saccades occurred.
Note:
-
Eye movements may be saccadic if you are moving your finger too fast. Slow the speed of your finger to see it the person can follow smoothly
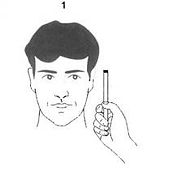
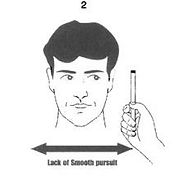
(Griessmeyer Law, 2011)
Saccadic Movements:
Procedure:
1. Instruct patient to keep head still.
2. Hold your finger/pen about 15 degrees to one side of your nose.
3. Ask the patient to look at your finger and then at your nose several times. Perform this left, right, up and down.
Look for:
-
The number of eye movements it takes for the patient’s eyes to reach the target, normal is less than 2.
-
Abnormal is several small movements or a big movement and overshoot.
Skew Deviation:
Procedure:
1. Instruct patient to keep head still.
2. Cover one eye.
3. Switch the cover from one eye to the other eye.
Look for:
-
A vertical corrective movement of the eye as it is uncovered
Note:
-
Effect of direction of gaze on the skew deviation
-
Any spontaneous tilt of the head and the effect of tilt on the skew deviation
VOR Cancellation/Suppression:
Procedure:
1. While seated, the patient is asked to extend their arms directly in front of their body and clasp their hands together with thumbs abducted and pointed towards the ceiling
2. The patient is then asked to visually fixate on their own thumbs and maintain that fixation
3. The patient’s entire body is then rotated from side to side. The rotation should cover an angle sweep of roughly 30 degrees to either side of the starting position.
Look for:
-
The normal response to the VOR cancellation test is for the eyes to remain stationary and motionless in the primary position of gaze throughout the middle of each side-to-side pass.
-
An abnormal response is for the patient to develop repetitive refixations during the middle of each rotational pass.
Note:
-
This whole-body rotation is most easily accomplished using a swivel chair, although it can also be approximated by asking the patient to twist at the waist from a stationary seat.
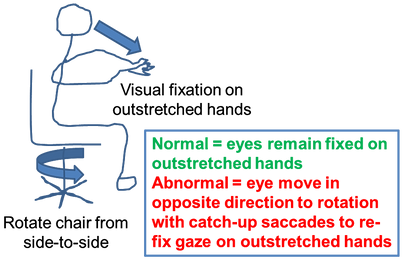
(Giovannoni, 2011)
Head thrust:
Procedure:
1. Inform the patient that you will be moving their head very quickly, but only through a small range.
2. Grasp patient’s head firmly with both hands on the sides of the head
3. Tilt the head forward 30 degrees so that the horizontal semicircular canal is level in the horizontal plane.
4. Instruct the patient to look at your nose.
5. Move the patient’s head side to side slowly, making sure the patient is relaxed.
6. Then, suddenly move the patient’s head in one direction and stop. The head movement should be small amplitude with the position held at the end.
Look for:
-
Patient’s ability to maintain visual fixation
-
Corrective saccades to re-fixate to your nose, noting the direction of head movement that caused re-fixation saccades.
Note:
-
If the patient has pain or significant restriction of cervical movement, the test should be performed with extreme caution or deferred.

(Look for Diagnosis, 2014)
Dynamic visual acuity:
Procedure:
1. Patient sits the appropriate distance from the acuity chart, wearing their glasses if they need distance correction.
2. Patient reads to the lowest line that they can until they cannot correctly identify all the letters on a given line.
3. Note the line where this occurs and the number of letters the patient incorrectly identifies.
4. Standing behind the patient, grasp patient’s head firmly with both hands on the sides of the head.
5. Tilt the head forward 30 degrees so that the horizontal semicircular canal is level in the horizontal plane.
6. While moving the patient’s head side to side at a frequency of about 2 complete side to side cycles per second, through a ROM of 1-2 inches in each direction, (so as to not restrict the visual field which may occur in patients who wear glasses) ask them to read to the lowest line that they can until they cannot correctly identify all the letters on a given line.
7. Note the line and where this occurs and or the number of incorrect letters.
Note:
-
A difference of less than or equal to 2 lines is normal.
-
A difference of greater than or equal to 3 lines is abnormal. (likely vestibular deficit)
-
If the patient has restriction of the cervical movement which limits your ability to perform the head movement the test cannot be properly performed and should be ceased.
Vertebrobasilar Insufficiency (VBI) test:
Purpose:
The vertebral artery test is used to test the vertebral artery blood flow, searching for symptoms of vertebral artery disease (Mitchell, 2007). A reduction of blood flow may result in a transient ischiamic attack (TIA).
Procedure:
1. Grasp patient’s head firmly with both hands on the sides of the head
2. Rotate head to EOR on one side maximally and holds position for 10 seconds, asking patient to report any symptoms.
3. Return to neutral for 10 seconds.
4. Repeat 2 in opposite direction.
5. Return to neutral for 10 seconds.
Look for:
-
Positive symptoms include dizziness, diplopia, dysarthria, dysphagia, drop attacks, nausea and vomiting, sensory changes and nystagmus.
Note:
-
If VBI test is positive do not complete hall pike and roll tests.

(Physical Therapy Nation, 2013)
Dix-Hallpike:
Contraindications: Disc Prolapse, cervical injury/trauma/fracture, cervical myelopathy/radiculopathy, dissection carotid/vertebral artery, positive VBI test
Procedure:
1. Patient long sits on the examination table and head is rotated 45 degrees
2. The head and trunk are quickly taken straight back so that the head is over the edge of the examination table by 20 degrees.
3. Hold for 30 seconds, observing for nystagmus and question for vertigo.
4. Patient is then brought up slowly to a sitting position with the head maintained in 45 degrees rotation.
5. Again, observe for nystagmus and question for vertigo.
6. Test is repeated with head rotated 45 degrees in opposite direction.
Look for:
-
Nystagmus, noting direction, latency, and duration.
Note:
-
A positive test indicates that BPPV is present.
-
If a positive result has been seen after step 3, progressing straight to Epley’s from that position is advisable.

(New Health Advisor, 2014)
Head roll test:
Contraindications: As Dix-Hallpike
Procedure:
1. Patient lies supine with the head flexed 20 degrees.
2. The head is turned quickly to one side.
3. Hold for 30 seconds, observing for nystagmus and question for vertigo.
4. Roll the head slowly back to the supine position, hold for 30 seconds.
5. Roll the head quickly to the other side.
6. Observe for nystagmus and question for vertigo.
Look for:
-
Observe nystagmus, noting direction, latency and duration.
-
Ask the patient which side is worse.
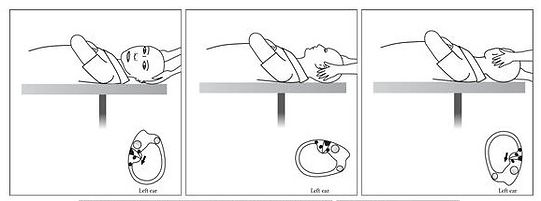
(Hornibrook, 2011)
Position Tests
It’s also important to perform any positional tests that have been reported by the patient to exacerbate symptoms; these can include but are not limited to:
-
Head turns
-
Head to knee
-
Sit to supine
-
Supine to sit
-
STS
-
Standing turns
Gait and Balance Assessments
Vestibular conditions often have a negative impact on balance and gait; therefore, specific tests of these areas should also be completed where appropriate. Examples of some appropriate tests:
-
6 minute walk test
-
6m walk test
-
TUG
-
Step test
-
CTSIB
-
Observation of gait
-
Positional BP